What Is Lyme Disease?
Lyme disease is an infectious disease primarily caused by the bacterium Borrelia burgdorferi and, to a lesser extent, Borrelia mayonii. Transmission to humans occurs through the bite of infected black-legged ticks, also widely referred to as deer ticks. These ticks most commonly become carriers of the bacteria after feeding on infected hosts, typically small mammals like mice and larger animals such as deer. The cycle of infection begins when these ticks, in their nymphal or adult stages, attach to the human body, often hiding in hard-to-see areas like the scalp, armpits, or groin.
 This disease is most prevalent in forested areas and grassy landscapes, where these ticks are more likely to come into contact with humans. The risk of contracting Lyme disease increases during warmer months when people are more likely to engage in outdoor activities and ticks are more active. As such, it is a significant public health concern in various regions, notably in the northeastern and upper midwestern United States, where these ticks are endemic.
This disease is most prevalent in forested areas and grassy landscapes, where these ticks are more likely to come into contact with humans. The risk of contracting Lyme disease increases during warmer months when people are more likely to engage in outdoor activities and ticks are more active. As such, it is a significant public health concern in various regions, notably in the northeastern and upper midwestern United States, where these ticks are endemic.
Early diagnosis and treatment of Lyme disease are crucial. If left untreated, the bacteria can spread throughout the body, leading to more severe symptoms and health complications over time, including neurological disorders, chronic joint inflammation, and heart rhythm issues. The initial stage is often marked by the appearance of a characteristic bull's-eye rash, known as erythema migrans, and flu-like symptoms. These indicators, combined with knowledge of potential tick exposure, form the basis for clinical diagnosis, which can be further supported by laboratory testing. Lyme disease's complexity and the severe implications of delayed treatment underscore the importance of preventive measures, such as using insect repellent, performing regular tick checks, and managing tick habitats in residential areas.
Symptoms and Stages of Lyme Disease
Lyme disease can present a range of symptoms, depending on the stage of the infection:
Symptoms of Lyme disease usually start 1–30 days after the tick bite.
The early stages of Lyme disease can be broken down into two phases: early localized Lyme disease and early disseminated Lyme disease. Recognizing the signs and symptoms of these stages is crucial for prompt treatment, which can prevent the disease from progressing to more severe stages.
Early Localized Lyme Disease
This stage occurs shortly after the tick bite, typically within 1 to 30 days. The primary symptom to look for is:
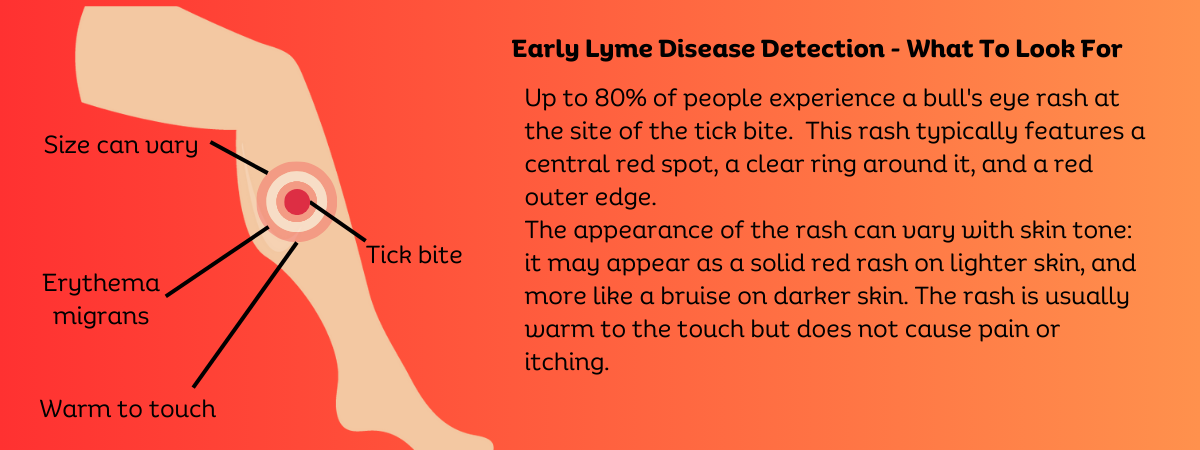
The Erythema Migrans rash, a hallmark sign of Lyme disease, is often recognized by its distinctive "bull's-eye" pattern. This notable pattern features a central red spot, which is surrounded by a clear, unblemished ring and then encircled by a larger ring of redness. Typically, this rash emerges at the location of the tick bite that transmitted the infection. Although the rash is neither itchy nor painful, it may feel unusually warm to the touch. It's important to recognize that while this rash is considered a classic indicator of Lyme disease, it does not appear in all infected individuals. Approximately 70-80% of those infected with Lyme disease will exhibit this rash, underscoring its significance in diagnosis but also highlighting that its absence does not rule out the disease. Awareness and timely recognition of this rash, along with other symptoms, are crucial for early diagnosis and effective treatment of Lyme disease.
Other symptoms during this stage can include:
- Fever
- Chills
- Headache
- Fatigue
- Muscle and joint aches
- Swollen lymph nodes
These symptoms can be quite mild and may not necessarily prompt an individual to seek medical attention immediately.
Early Disseminated Lyme Disease
This stage occurs weeks to months after the tick bite when the bacteria begin to spread throughout the body. Symptoms during this stage are more diverse and can affect multiple systems:
Multiple Erythema Migrans Rashes: Additional rashes may appear on different areas of the body, distinct from the original tick bite site.
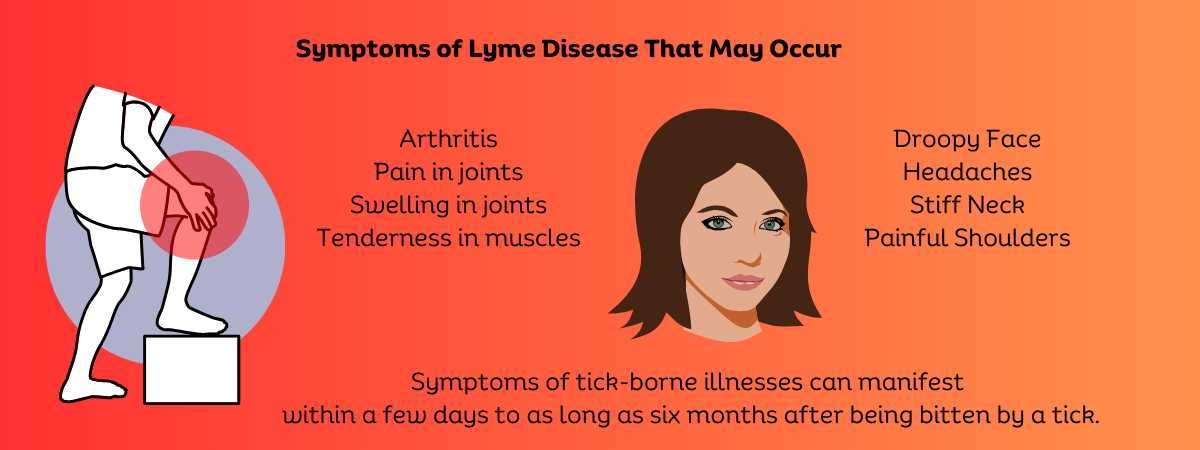
Neurological Symptoms: Lyme disease can lead to several severe neurological complications if not adequately treated. These may include facial palsy, which manifests as weakness or drooping on one or both sides of the face, often resulting in a significant loss of facial muscle control. This condition can affect a person's ability to express emotions visually and can impair basic functions such as blinking and smiling.
Additionally, symptoms akin to those of meningitis, another serious consequence of Lyme disease, can develop. These symptoms include a severe headache, profound neck stiffness, and an increased sensitivity to light, all of which suggest inflammation of the protective membranes covering the brain and spinal cord. Such symptoms require immediate medical attention as they can indicate serious progression of the infection.
Radiculopathy is also a common neurological issue associated with Lyme disease, characterized by pain, weakness, or numbness in the limbs. This occurs when nerve roots exiting the spine become inflamed or compressed, and can significantly impact mobility and quality of life, making everyday activities challenging.
These symptoms highlight the critical nature of Lyme disease as a multi-systemic condition that can severely affect neurological health. The diverse and impactful nature of these symptoms underscores the need for prompt diagnosis and treatment to prevent long-term damage and ensure a better health outcome. Recognizing and addressing these symptoms early can significantly reduce the risk of chronic health issues and improve the overall prognosis for affected individuals.
Cardiac Symptoms: Less common but potentially serious symptoms include Lyme carditis, which can manifest as palpitations, chest pain, or lightheadedness due to changes in heart rhythm.
Early Localized Stage: This initial stage occurs a few days to a month after the tick bite. The most recognizable symptom is the erythema.
The early localized stage of Lyme disease occurs shortly after a tick bite, usually within 1 to 30 days. This phase is characterized primarily by the appearance of the erythema migrans rash, which is one of the most notable signs of Lyme disease. Here are the key features of this stage:
What Is The Erythema Migrans Rash?
Appearance: The rash associated with Lyme disease typically starts as a small red spot at the site of the tick bite. Over a period of days or weeks, this initial mark may expand, developing into a larger circular or oval-shaped rash. As it grows, the rash often clears in the center, which can result in the distinctive bull's-eye pattern that is commonly associated with Lyme disease. However, it's important to note that this classic bull's-eye appearance is not always present. The variability in its manifestation means that the rash can take on several forms, which can sometimes complicate the diagnosis. Awareness of the potential for different presentations of the rash is crucial for prompt and accurate identification and treatment of Lyme disease.
Location: Can appear anywhere on the body, not just at the site of the tick bite.
Symptoms: The rash is typically not itchy or painful but might feel warm to the touch.
Other Symptoms
Aside from the rash, the early localized stage of Lyme disease can also include:
- Fever
- Chills
- Headache
- Fatigue
- Muscle and joint aches
- Swollen lymph nodes
These symptoms are often mild and can be mistaken for those of common viral infections, which sometimes leads to underdiagnosis or misdiagnosis.
Importance of Early Diagnosis
The early localized stage of Lyme disease is critical for accurate recognition and timely diagnosis, which are essential for effective treatment outcomes. Administering the appropriate antibiotics, such as doxycycline, amoxicillin, or cefuroxime axetil, promptly at this stage usually results in complete recovery for most individuals. Early intervention not only mitigates the immediate symptoms but also plays a crucial role in preventing the disease from advancing to more severe, disseminated stages. Without prompt treatment, Lyme disease can progress and spread to various parts of the body, leading to more complex health issues involving the joints, nervous system, and heart. Therefore, early detection and treatment are paramount to halt the progression of the disease and ensure a full recovery, minimizing the risk of long-term complications.
Late Disseminated Stage:
The Late Disseminated Stage of Lyme disease represents a more advanced phase of the infection, which can develop if the disease remains untreated. This stage typically occurs months to years after the initial tick bite. During this phase, patients may experience severe symptoms that affect multiple body systems. One of the most common manifestations is Lyme arthritis, which involves significant joint pain and swelling, especially in the knees. Additionally, neurological complications are frequent, including symptoms such as numbness, tingling, and shooting pains that can affect the arms or legs. Cognitive impairments, such as memory loss or difficulty concentrating, are also reported, reflecting the potential impact of the disease on brain function.
These symptoms illustrate the systemic nature of late-stage Lyme disease, as the bacteria spread and cause inflammation in various parts of the body. The progression to this stage underscores the importance of early diagnosis and treatment to prevent long-term health issues and improve outcomes for those affected by Lyme disease.
Symptoms of Late Disseminated Lyme Disease
The symptoms in this stage can affect multiple body systems and include:
Arthritis: One of the hallmark symptoms of late disseminated Lyme disease is Lyme arthritis, characterized by significant pain and swelling predominantly in the large joints, with the knees often being the most affected. This condition may manifest as intermittent episodes of arthritis, where symptoms can flare up periodically and then subside. Over time, without appropriate and timely treatment, these bouts of arthritis can potentially evolve into a chronic condition, causing persistent discomfort and potentially leading to long-term joint damage. This progression underscores the importance of early detection and intervention in Lyme disease to prevent its advance to this debilitating stage.
Neurological Problems:
When Lyme disease progresses without adequate treatment, the bacteria can profoundly affect the nervous system, leading to a range of serious conditions. One such condition is encephalopathy, a brain disorder that can impair cognitive functions. Individuals suffering from encephalopathy due to Lyme disease may experience memory loss, significant difficulties with concentration, and challenges in processing information, often described colloquially as "brain fog." This cognitive decline can severely impact daily functioning and quality of life.
Additionally, Lyme disease can cause other severe neurological symptoms. For instance, neuropathy, which manifests as pain, weakness, and numbness in the hands and feet, can occur when the peripheral nerves are damaged. Another common neurological manifestation is facial palsy, specifically Bell’s palsy, where there is paralysis or severe weakness of the facial muscles. This can result in a drooping appearance on one or both sides of the face and can affect facial expressions and the ability to close the eyelids.
These neurological effects highlight the critical nature of Lyme disease as a multi-systemic infection that can lead to significant, sometimes irreversible damage if not diagnosed and treated promptly. The potential for such severe complications emphasizes the need for awareness and timely medical intervention.
Heart Problems: While it is less frequently encountered, Lyme carditis is a serious complication that can arise during the dissemination stage of Lyme disease. This condition impacts the heart's electrical conduction system, potentially leading to cardiac conduction disturbances like atrioventricular (AV) block. When the electrical signals between the chambers of the heart are impeded or slowed significantly, patients may experience a range of symptoms. These can include palpitations, where the heart feels like it is beating too hard or too fast, dizziness, and shortness of breath. Chest pain is also a possible symptom. Such manifestations necessitate immediate medical evaluation, as Lyme carditis can be life-threatening if not promptly and effectively treated.
Additional Erythema Migrans Rashes: In some cases, new erythema migrans rashes may appear in other areas of the body.
Other Symptoms: Persistent fatigue, headaches, and sleep disturbances are also commonly reported by individuals in the late disseminated stage.
Diagnosis and Treatment
Diagnosing Lyme disease in the late disseminated stage can be challenging, as the symptoms are often similar to those of other chronic conditions. Diagnosis usually involves a combination of medical history, symptom assessment, physical findings, and laboratory tests to detect antibodies to the Lyme bacteria. However, testing can sometimes yield false negatives in this stage.
Treatment typically involves longer courses of antibiotics, which may be given orally or intravenously, depending on the severity and the specific symptoms presented. In cases of Lyme arthritis, anti-inflammatory treatments might also be used to manage symptoms. Neurological and cardiac symptoms may require specialized treatments and ongoing management.
Prognosis
The prognosis for late disseminated Lyme disease can vary. While many people eventually recover after appropriate antibiotic treatment, some may continue to experience symptoms long after the infection has been eradicated, a condition known as Post-Treatment Lyme Disease Syndrome (PTLDS). This syndrome can lead to significant chronic pain, fatigue, and cognitive dysfunction, affecting quality of life.
Prompt recognition and treatment of Lyme disease in its early stages is the best way to prevent progression to late disseminated Lyme disease. If you suspect you have Lyme disease at any stage, it's crucial to seek medical care promptly to discuss your symptoms and potential treatment options.
How Is Lyme Disease Diagnosed?
The diagnosis of Lyme disease primarily relies on clinical evaluation, which includes an assessment of symptoms, physical signs such as the characteristic rash, and a review of the patient's potential exposure to infected ticks. To further substantiate the diagnosis, healthcare providers often turn to laboratory testing. These tests usually involve blood analyses designed to detect antibodies produced by the body in response to the Borrelia burgdorferi bacteria. Confirming the presence of these antibodies through tests like the ELISA (Enzyme-Linked Immunosorbent Assay) followed by Western blot testing helps to verify the diagnosis, especially in cases where symptoms are ambiguous.
Natural Herbs For Lyme disease
In his book "Healing Lyme Disease," Stephen H. Buhner explores natural methods for tackling Lyme disease. He provides a comprehensive guide on various notable herbs, detailing the specifics of how, when, where, and why to use these herbs and supplements effectively in the treatment process.
Here are some herbs that are often cited for their potential benefits in supporting the treatment of Lyme disease:
- Cat’s Claw (Uncaria tomentosa): Often used for its anti-inflammatory and immune-boosting properties, cat’s claw may help reduce some of the inflammation associated with Lyme disease and support the immune system.
- Garlic (Allium sativum): Known for its antimicrobial effects, garlic is thought to help fight infections, although its effectiveness specifically against Borrelia burgdorferi (the bacteria that causes Lyme disease) in humans needs more research.
- Andrographis (Andrographis paniculata): This herb is popular in traditional Chinese and Indian medicine. It is known for its antimicrobial and anti-inflammatory properties and is often used in herbal protocols for Lyme disease.
- Japanese Knotweed (Polygonum cuspidatum): Rich in resveratrol, Japanese knotweed is used for its anti-inflammatory and antioxidant properties. It is also thought to protect blood vessels and reduce symptoms related to inflammation.
- Turmeric (Curcuma longa): Known for its potent anti-inflammatory effects due to its curcumin content, turmeric may help reduce inflammation caused by Lyme disease.
- Huang Qin (Scutellaria baicalensis): Properties: Huang Qin is known for its anti-inflammatory, antibacterial, and antiviral properties. It contains baicalin, a flavonoid that has been shown to help reduce inflammation and support immune function.
- Dan Shen (Salvia miltiorrhiza): Properties: Dan Shen is known for its ability to improve circulation and reduce inflammation. It has antioxidant properties and is commonly used in traditional Chinese medicine to treat blood circulation disorders and as a heart tonic.
Use in Lyme Disease: Dan Shen might help manage cardiovascular symptoms that can appear in later stages of Lyme disease, such as Lyme carditis. It’s thought to aid in improving blood flow and reducing inflammation. - Fang Ji (Stephania tetrandra): Properties: This herb is traditionally used to reduce pain and inflammation. Fang Ji is often employed in traditional medicine to treat conditions involving water retention and inflammation. Use in Lyme Disease: It could potentially help alleviate joint pain and swelling, which are common symptoms of Lyme arthritis.
- Xu Duan (Dipsacus asper): Properties: Xu Duan is traditionally used to strengthen bones and sinews, promote blood circulation, and reduce pain. It’s often recommended in traditional Chinese medicine for healing fractures, strengthening the tendons and bones, and for back and leg pain. Use in Lyme Disease: Given its properties, Xu Duan might be useful in managing musculoskeletal symptoms associated with Lyme disease, such as joint pain and muscle aches.
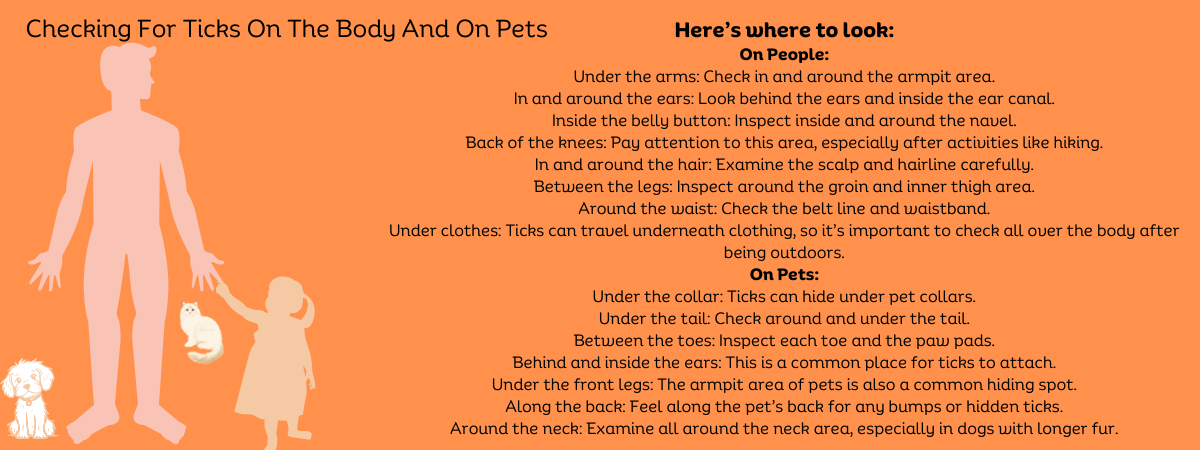
Prevention
Preventive measures include using insect repellent, wearing long sleeves and pants, avoiding wooded and bushy areas with high grass, and performing thorough tick checks after spending time outdoors in areas where ticks are common. Prompt removal of ticks is also crucial to prevent infection.
Lyme disease is the most common tick-borne illness in the United States, particularly in the Northeast and upper Midwest. Awareness and early treatment are key to effectively managing Lyme disease and preventing its long-term complications.
What If I Get A Tick On Me?
If you get bitten by a tick, it's crucial to remove it promptly. The Centers for Disease Control and Prevention (CDC) recommends the following steps for tick removal:
Use a pair of tweezers to grasp the tick as close to the skin's surface as possible.
Pull upward with steady, even pressure. Avoid twisting the tweezers, as this can cause parts of the tick to break off and remain embedded in the skin.
Once the tick is removed, thoroughly clean the bite area with soap and water or rubbing alcohol.
Avoid crushing the tick. Dispose of it by placing it in alcohol, flushing it down the toilet, or sealing it in a bag and discarding it in the trash.
How To Make Your Yard Tick Free
Creating a tick-free garden involves several strategies to reduce the presence of ticks and minimize the risk of tick-borne diseases like Lyme disease. Here are some effective steps you can take to make your garden less attractive to ticks:
1. Keep Your Lawn Mowed and Well-Maintained
Ticks thrive in tall grass and overgrown vegetation. Regularly mowing your lawn and keeping grass short reduces the habitat ticks prefer.
2. Clear Tall Grasses and Brush
Remove tall grass and brush around the home and at the edge of the lawn. This also reduces the tick habitat and makes the boundary less inviting for ticks.
3. Create a Tick Barrier
Use a three-foot-wide barrier of wood chips or gravel between your lawn and wooded areas to restrict tick migration into recreational areas. Ticks are less likely to cross this type of barrier because it exposes them to drier, less favorable conditions.
4. Discourage Wildlife Hosts
Ticks often enter your yard by hitching a ride on wildlife like deer, rodents, and birds. Use fencing to discourage deer from entering your yard, and keep bird feeders away from the house as they can attract ticks from bird visitors.
5. Keep Ground Under Bird Feeders Clean
Bird feeders can attract rodents which can carry ticks. Regularly cleaning up spilled seeds and debris under bird feeders will help reduce the attraction for rodents.
6. Use Tick-Repelling Plants
Planting tick-repelling plants around your yard can help keep ticks away. Examples of such plants include garlic, rosemary, lavender, and marigolds, which are known for their natural tick-repellent properties.
7. Maintain a Clean Yard
Keep your yard free of clutter where ticks can hide. Remove leaf litter, tall weeds, and stack wood neatly and in a dry area to discourage rodent activity that can attract ticks.
Frequently Asked Questions About Lyme Disease
Here are six commonly asked questions about Lyme disease, along with their answers:
-
What is Lyme disease? Lyme disease is a bacterial infection transmitted to humans through the bite of infected black-legged ticks, commonly known as deer ticks. The bacteria responsible for the disease is Borrelia burgdorferi.
-
What are the symptoms of Lyme disease? Early symptoms of Lyme disease include fever, headache, fatigue, and a characteristic skin rash called erythema migrans, which often appears as a bull's eye pattern. If untreated, the infection can spread to the joints, heart, and nervous system.
-
How is Lyme disease diagnosed? Lyme disease is diagnosed based on symptoms, physical findings (like the rash), and the possibility of exposure to infected ticks. Laboratory tests are most helpful in the later stages of the disease and can confirm the diagnosis through tests such as ELISA and Western blot, which detect antibodies to the bacteria.
-
Can Lyme disease be treated? Yes, Lyme disease is treatable. The standard treatment is natural remedies, antibiotics, typically doxycycline, amoxicillin, or cefuroxime axetil. Treatment is most effective when started early.
-
Is Lyme disease preventable? Lyme disease can be prevented by avoiding tick-infested areas, using insect repellent, wearing protective clothing, performing thorough tick checks after being outdoors, and promptly removing ticks with tweezers.
-
Can Lyme disease be cured? Most cases of Lyme disease can be cured with a 2-4 week course of oral antibiotics. In some cases, symptoms like pain, fatigue, or cognitive difficulties might persist even after treatment, a condition known as Post-Treatment Lyme Disease Syndrome (PTLDS). However, long-term outcomes are generally good with appropriate treatment.
Summary Of Lyme Disease
Lyme disease is a bacterial infection caused by the bacterium Borrelia burgdorferi, which is transmitted to humans through the bite of infected black-legged ticks, often called deer ticks. The most recognizable early sign of Lyme disease is a skin rash known as erythema migrans, which typically appears as a bull's eye pattern—red at the center, surrounded by a clear ring and another circle of redness. Other early symptoms include fever, headache, and fatigue. If left untreated, the infection can spread to joints, the heart, and the nervous system, leading to more severe health problems.
Diagnosis is based on symptoms and the likelihood of tick exposure, supported by laboratory tests in later stages of the disease. Lyme disease is treatable with natural remedies, and antibiotics, like doxycycline, amoxicillin, or cefuroxime axetil commonly prescribed. Early treatment usually leads to a full recovery, although some individuals might experience lingering symptoms known as Post-Treatment Lyme Disease Syndrome (PTLDS).
Prevention strategies include avoiding tick-infested areas, using insect repellents, wearing protective clothing, and conducting thorough tick checks after outdoor activities. Proper tick removal techniques are crucial to prevent infection after a tick bite.
References:
https://www.cdc.gov/lyme/index.html
https://www.mayoclinic.org/diseases-conditions/lyme-disease/symptoms-causes/syc-20374651
https://en.wikipedia.org/wiki/Lyme_disease
https://my.clevelandclinic.org/health/diseases/11586-lyme-disease
https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/lyme-disease
https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/LymeDisease.aspx
https://www.fda.gov/consumers/consumer-updates/ticks-and-lyme-disease-symptoms-treatment-and-prevention
https://lymediseaseassociation.org/category/book-list/
https://www.lymedisease.org/top-12-lyme-books-diamond/
https://www.lymenet.org/books.shtml

